Does Diabetes Affect Your Mental Health?
Navigate the intersection of diabetes and mental health with insights on managing both. Discover strategies to support emotional well-being while effectively managing diabetes for a balanced and fulfilling life.

According to the Diabetes Research Institute, over 34 million people are living with diabetes in the U.S. alone; while The World Health Organization (WHO) reports that over 422 million people worldwide live with Diabetes mellitus. Where so many people are affected with this disease; there are a couple of questions, which bug every diabetes patient – Does diabetes affect my mental health? Are diabetes and mental health connected?
Contents
What is Diabetes?
Diabetes mellitus, commonly known as diabetes, is a metabolic disease that causes high blood glucose (sugar) levels persisting over a prolonged period of time. Type 1 diabetes is a disease where the body doesn’t make any insulin at all. The body’s immune system destroys the cells in the pancreas that produce insulin, a hormone used by the body to keep blood glucose levels in check. Type 2 diabetes, caused by dietary and other environmental factors, is a condition in which the pancreas makes some insulin but not enough; or the body cells become overwhelmed by insulin and fail to properly respond; they become resistant to insulin.
Diabetes And Mental Health connection
When we talk impact of diabetes on our body, its physical manifestations and symptoms often come to our mind first. After all, the cardiovascular problems, vision impairment, hypertension, foot complications, and high risk of wound infection due to slower healing weigh heavy on the minds of those with diabetes and their caregivers. However, diabetes affects people in a more insidious way that is no less important – it impacts mental health.
Think about it. There is one more physical part of body – That’s brain; which gets directly affected by diabetes mellitus. Diabetes is characterized by blood glucose (sugar) levels that are too high. The brain functions, which include thinking, judgment, memory, learning, emotions, and behavior are closely linked to glucose levels and how efficiently the brain uses this fuel source. If you have too much glucose coursing through your body, your brain will be affected along with your eyes, skin, feet, and every other anatomical system.

Diabetes Management for Better Mental Health
Existing diabetes, whether it be type 1 diabetes or type 2 diabetes; can make mental health conditions worse. Here are the tips to manage Diabetes for better mental health.
Increase Your Knowledge
Diabetes management requires awareness. Learning more about diabetes can help you maintain a positive attitude and practice proper diabetes self-management. Know what makes your blood sugar level rise and fall — and how to control these day-to-day factors. By understanding more about diabetes and blood sugar control, you will be able to make necessary lifestyle changes.
You may join a diabetes education group or online diabetes support communities. You can also talk to other people with diabetes. Other people with diabetes understand some of the things you are going through. Ask them how they deal with their diabetes and what works for them.
Eat at regular intervals

Meal timing play an important role for diabetic patients. Take small portions at regular intervals. As a general rule, try to minimize any long gaps during the day without eating. Don’t skip meals, skipping a meal can lead to immediately dangerous blood sugar swings, as well as potential complications down the road. If you are on medications to reduce your sugar levels and you skip a meal, it may lead to hypoglycemia.
Cut out sweet beverages
When it comes to successfully managing type 2 diabetes, what you drink is just as important as what you eat. There’s an astounding level of sugar in juices, sodas, and other sweet drinks. By replacing these beverages with water, you’ll be making a giant step in the right direction.
Anything that’s liquid that has carbohydrates will digest faster than something you would have to chew. The result: a quick spike in blood sugar.
Pay attention to all types of sugar
When reading nutrition labels, it’s important to pay attention to all varieties of sugar. Fructose, dextrose, corn syrup, honey, lactose, raw sugar, and sucrose are a few fairly common sugar types.
Switch to healthy snacks
Instead of sweet treats like cookies and candy, try grabbing fresh fruits, roasted nuts or vegetables.
Here are best snack ideas, if you have diabetes
- Hard-Boiled Eggs
- Homemade Protein Bars
- Yogurt with Berries
- Handful of Almonds
- Egg Muffins
- Veggies and Hummus
- Avocado
- Turkey Roll-Up
- Chia Seed Pudding
- Peanut Butter Celery Sticks
- Trail Mix
- Tuna Salad
- Black Bean Salad
- Sliced Apples with Peanut Butter
- Cottage Cheese
- Edamame
- Roasted Chickpeas
- Cheese and Whole-Grain Crackers
- Popcorn
- No-Bake Energy Bites
Be more observant
Because sugar tastes good; food manufacturers tend to add more sugar than necessary to processed foods. By checking labels, you can help familiarize yourself with products that contain too much sugar. Common culprits include breads, sauces, and dressings.
Exercise

Physical activity or exercise is an inherent part of every diabetes management plan. Exercise can help your body counter the negative effects of an unhealthy diet. It encourages healthy functions throughout your whole body. When it comes to sugar, burning that energy through physical activity can mitigate sugars’ negative impact. When you exercise, your muscles use sugar (glucose) for energy. Regular physical activity also helps your body use insulin more efficiently.
These factors work together to lower your blood sugar level. The more strenuous your workout, the longer the effect lasts. But even light activities — such as housework, walking, gardening or being on your feet for extended periods — can improve your blood sugar.
Alcohol
Moderate amounts of alcohol consumption can cause a rise in blood sugar, while excessive alcohol consumption can have the reverse effect. Too much alcohol can cause a dangerous drop in blood sugar levels and can have the same impact on healthy brain and body functions. The liver normally releases stored sugar to counteract falling blood sugar levels. But if your liver is busy metabolizing alcohol, your blood sugar level may not get the boost it needs from your liver. Alcohol can result in low blood sugar shortly after you drink it and for as long as 24 hours afterward.
Keep a count of your alcohol consumptions and don’t drink alcoholic beverages on an empty stomach.
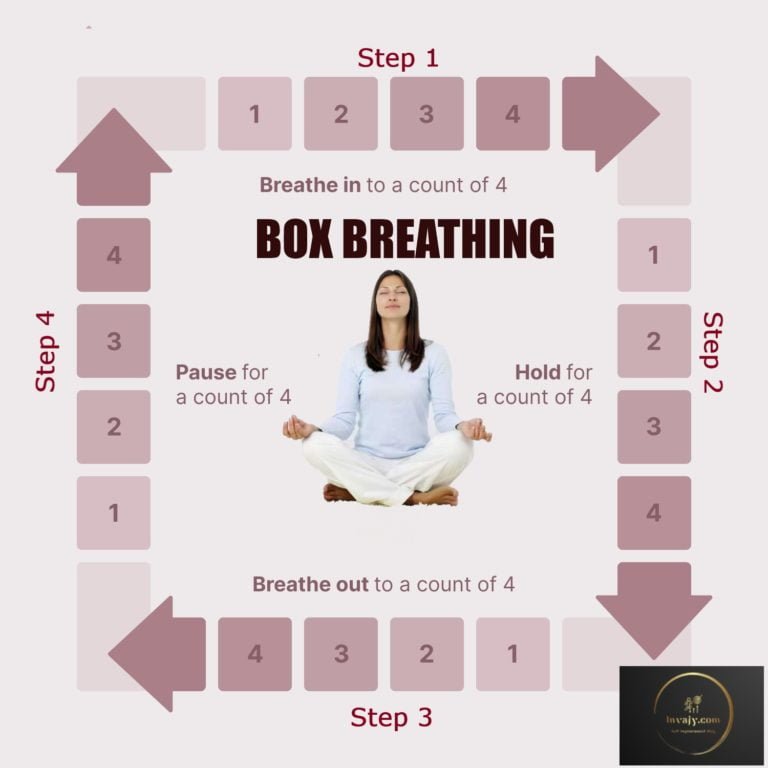
Stress
If you’re stressed, the hormones your body produces in response to prolonged stress may cause a rise in your blood sugar level. Additionally, it may be harder to closely follow your usual diabetes management routine if you’re under a lot of extra pressure. Spot your stress warning signs and take action to prevent stress and keep your blood sugar low. Try to reduce your stress level try deep breathing, gardening, taking a walk, meditating, working on your hobby, or listening to your favorite music.
Medication
Insulin and other diabetes medications are designed to lower your blood sugar levels when diet and exercise alone aren’t sufficient for managing diabetes. But the effectiveness of these medications depends on the timing and size of the dose. Follow the medication advice of your medical practitioner and take the prescribed doses on time. Skipping your medicine or not taking them at prescribed time may increase the blood sugar levels.
Routine Checkups
See your health care team at least twice a year to find and treat any problems early. At each visit, be sure you have a tests and check like A1C test, cholesterol test, blood pressure check, eye test, BMI check and foot check.
Also buy glucometer and do self-check of your sugar levels at home regularly. Maintain a Diabetic Care Record, which will help you and your doctors in managing the disease.
Get Enough Sleep

Not getting enough sleep can have a major impact on your blood sugar levels. Decreased sleep is a risk factor for increased blood sugar levels. Even partial sleep deprivation over one night increases insulin resistance, which can in turn increase blood sugar levels. Try to get at least six to eight hours of sleep per night. Some great tips that help with falling asleep are limiting exposure to blue light from phones or other screens close to your bedtime as well as limiting caffeine intake during the day. If you still have trouble sleeping, talk to your health care provider for advice.
I hope, if you will use above tips and strategies for diabetes management; you will surely be able to manage improve your mental health conditions in a better way.
That’s all from my side. I hope, you liked this article on diabetes care for better mental health. Please share this on your favorite social media portals with your friends and relatives.
(Disclaimer: This article is for general information only. Before adopting preventive methods/measures/treatment, please seek medical advice.)